American College Of Sports Medicine Guidelines Exercise Program
American College of Sports Medicine Recommendations and Position Stand ExRx.net Weigh Training Outline Recommendations for Resistance Training Exercise (ACSM 1995). Provides the tools and scientific evidence needed to create safe and effective exercise programs. It also acts as the official preparation. Designed as a companion to ACSM's Guidelines for Exercise Testing and Prescription, Recommended for ACSM Certification Examinations! The single most internationally read and.
American College Of Sports Medicine Guidelines Exercise Program Printable
Abstract
In 2009, the American College of Sports Medicine convened an expert roundtable to issue guidelines on exercise for cancer survivors. This multidisciplinary group evaluated the strength of the evidence for the safety and benefits of exercise as a therapeutic intervention for survivors. The panel concluded that exercise is safe and offers myriad benefits for survivors including improvements in physical function, strength, fatigue, quality of life (QOL), and possibly recurrence and survival. Recommendations for situations in which deviations from the US Physical Activity Guidelines for Americans are appropriate were provided. Here, we outline a process for implementing the guidelines in clinical practice, and provide recommendations for how the oncology care provider can interface with the exercise and physical therapy community.
INTRODUCTION
In oncology, there is a formal vetting process to introduce new standards of patient care. This process, managed by the National Comprehensive Cancer Network (NCCN) (nccn.org), produces evidence-based guidelines that are then implemented at the institution or practice level. While variations in practice remain, even within the context of the guidelines, they provide a standard of care and a process for defining evidence-based cancer care.
Medical and behavioral interventions have physiologic effects, which necessitate their evaluation for safety before widespread implementation. Through this evaluation, providers understand whether the purported benefits of an intervention truly exist and outweigh any risks. As exercise has physiologic effects, it can be considered a therapeutic intervention, as it has in other clinical settings (eg, cardiac rehabilitation). Until recently, evaluation of exercise as a therapeutic intervention in a cancer treatment and survivorship setting had not been undertaken. There is a need for an evaluation of the risks and benefits of exercise-based interventions for cancer survivors by a body that understands clinical medicine, oncology, and exercise.
The American College of Sports Medicine (ACSM) has a long history of providing this kind of evaluation, as the organization comprises clinicians, exercise physiologists, epidemiologists, behavioral scientists, and exercise specialists. As such, in 2009, the ACSM convened an expert panel to provide such an evaluation, and invited a multidisciplinary team of researchers and practitioners to evaluate the evidence and issue guidelines on exercise for cancer survivors.
ACSM GUIDELINES EXPERT PANEL
In 2009, with support from the Siteman Cancer Center and the Oncology Nursing Society, the ACSM convened an expert roundtable to review the literature on exercise in cancer survivors and issue guidelines for activity, along with recommendations on exercise testing and prescription. The target audience for the resulting document was the exercise professional who was expected to develop an exercise program for cancer survivors. Such programs would take into account where the survivors were in the cancer control continuum (eg, on active treatment, several years past diagnosis, with existing disease), as well as their current health status, and would assume that exercise professionals will work in conjunction with the survivors and cancer care teams as necessary. The assembled evidence was reviewed by the panel and graded based on National Heart, Lung, and Blood Institute (NHLBI) categories.3 The review was conducted for those tumor sites where sufficient evidence was available in adults: breast, prostate, colon, gynecologic, and hematologic. Data on exercise programs in children do exist, largely in hematologic cancers, but were not included, and have been reviewed elsewhere. The ACSM guidelines review included evaluation of the risk-benefit equation; the questions of both safety and benefits of exercise were considered. Survivors were defined according to the National Coalition for Cancer Survivorship recommendation, as “from the time of diagnosis until the end of life.”5
ACSM GUIDELINES ON EXERCISE FOR CANCER SURVIVORS
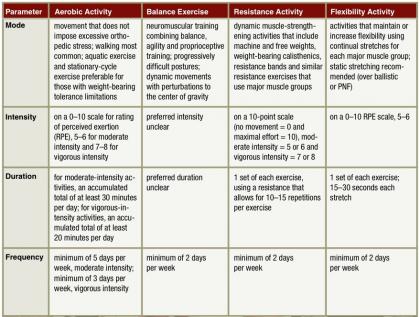
The ACSM physical activity guidelines for cancer survivors have at their foundation two existing documents. First, the US Department of Health and Human Services 2008 Physical Activity Guidelines for Americans (PAGA) provided direction with respect to the recommended types and amounts of physical activity.6 Second, the ACSM Guidelines for Exercise Testing and Prescription were relied upon to address safety issues for medical conditions other than those associated with cancer, as well as general principles for exercise prescription.7 PAGA notes that all individuals should strive to avoid inactivity, and that any level of physical activity may provide health benefits. The same recommendation was made for cancer survivors in the ACSM guidelines, with an emphasis on returning to normal daily activities as quickly as possible after surgery and continuing these activities as much as possible during any adjuvant treatments (Table 1). For adults to gain substantial health benefits, PAGA suggests at least 150 min/week of moderate-intensity activity or 75 min/week of vigorous-intensity activity (or an equivalent combination). Additional benefits are gained with greater amounts of activity. PAGA applies the same prescription to older adults, with the addition that those whose physical conditions preclude participation in 150 min/week of moderate-intensity activity, such as cancer survivors, should be as active as they are able. For resistance training, PAGA recommends moderate- or high-intensity activities for all major muscle groups at least twice per week. To improve flexibility, PAGA recommends that adults stretch major muscle groups and tendons on days they participate in other types of activity. PAGA also notes that older adults benefit from balance exercises.
Table 1
Summary of the ACSM Exercise Guidelines for Cancer Survivors.a
| Aerobic | Resistance | Flexibility | |
|---|---|---|---|
| US Physical Activity Guidelines for Americans (PAGA)b | 150 min/week of moderate-intensity or 75 min/week of vigorous-intensity activity, or an equivalent combination. | Muscle-strengthening activities of at least moderate intensity at least 2 days/week for each major muscle group. | Stretch major muscle groups and tendons on days other activities are performed. |
| Breast | Follow US PAGA. | Start with supervised program and progress slowly. | Follow US PAGA. |
| Prostate | Follow US PAGA. | Follow US PAGA. | Follow US PAGA. |
| Colon | Follow US PAGA. | Follow US PAGA except with stoma, where lower resistance and slower progression are recommended to avoid herniation. | Follow US PAGA, taking care to avoid excess abdominal pressure if patient has ostomy. |
| Gynecologic | Morbidly obese women may require additional supervision. | Data on safety and benefits are not available for women with lower limb lymphedema. | Follow US PAGA. |
| Hematologic, no HSCT | Follow US PAGA. | Follow US PAGA. | Follow US PAGA. |
| Hematologic with HSCT | Recommend starting with lighter intensity and slower progression to greater intensity and duration. | Follow US PAGA. Resistance training may have particular benefits in this population. | Follow US PAGA. |
For aerobic training, the ACSM guidelines for cancer survivors are to follow the age-appropriate PAGA recommendations. The ACSM guidelines note that modifications of varying degrees to PAGA are sometimes needed for many cancer survivors to safely participate in resistance training. Similarly, the ACSM guidelines for flexibility in cancer survivors are the same as those for all adults, with some modifications based on the survivors' condition. For example, the ACSM guidelines note that colon cancer survivors with ostomies should take care to avoid excessive abdominal pressure. Many other conditions may also require precautions, as with breast tissue expanders, peripherally inserted central catheter (PICC) lines, intraperitoneal catheters, and other postsurgical limitations.
IMPLEMENTING EXERCISE RECOMMENDATIONS IN CANCER SURVIVORS
The ACSM panel noted numerous potential benefits for exercise in the cancer survivor population (Table 2), which have also been summarized in other reports.– Exercise has the potential to improve physical function, aerobic capacity, strength, and flexibility. Data exist for a key role of exercise in maintaining a healthy body composition as well as a healthy body image. Exercise has benefits on quality of life (QOL), including fatigue, and may reduce the anxiety associated with recurrence. In addition to the documented benefits, ongoing research is exploring the role of exercise in prolonging disease-free survival and reducing risk of recurrence and death.– Exercise may improve survivors' ability, physically and psychologically, to complete treatment. Finally, exercise may reduce or prevent long-term and late effects of treatment.

Table 2
Rating the evidence-base supporting the ACSM Exercise Guidelines for Cancer Survivors. Adapted from Schmitz et al 2010.
| Breast (During) | Breast (After) | Prostate | Hematologic (During or After HSCT) | Hematologic (No HSCT) | |
|---|---|---|---|---|---|
| Safety | A | A | A | A | |
| Fitness | A | A | A | C | B |
| Strength | A | A | A | C | |
| Body composition | B | B | B | ||
| QOL | B | B | B | C | |
| Fatigue | B | B | A | C | B |
| Anxiety | B | B | |||
| Flexibility | A | ||||
| Physical function | A | B | |||
| Lymphedema | A (is safe) | ||||
| Body image | B |
The ACSM guidelines for survivors were written to be applicable to both clinical exercise physiologists who may be working within a cancer center, as well as exercise professionals who work in the community setting. Exercise professionals were encouraged to work with the cancer care team when necessary to understand the survivor's treatment and medical risks. Here, we outline what evaluations were recommended in those guidelines, and the kind of information that exercise professionals need from the clinical care team to develop a safe and effective exercise program for survivors, as well as the information that survivors need to exercise without supervision. Ideally, survivors would work with a certified exercise professional (for example, a trainer with ACSM Cancer Exercise Trainer certification) when they undertake a new exercise program. However, we recognize that numerous circumstances (eg, physical location, financial ability) may preclude this, and it should not serve as a barrier to a survivor following the key component of the guideline: Avoid inactivity. Thus, the clinical care team should be prepared to provide survivors with enough information to move safely, which nearly every survivor can do.
The rich evidence base that informed the ACSM guidelines shows that exercise is safe for survivors and that there are morbidities for which exercise is a useful therapeutic intervention. However, implementation of the guidelines among survivors poses challenges. Connecting survivors to appropriate programs and identifying survivors for whom community-based programs may not be appropriate remains a challenge. The ACSM guidelines detail considerations that might guide such decision making. However, one of the major challenges in this process is the lack of evidence-based thresholds for most of the clinical indicators that are recommended as considerations.
In clinical practice, thresholds for defining risk and safety are necessary for consistent care and are often implemented on an institution-specific basis, based on the clinical experience of a few individuals, particularly when the research base is limited or nonexistent. Such practices can be set without much evidence, but change only with substantial contrary evidence, and often only from large, randomized, controlled trials. Thus, setting thresholds and therapeutic intervention plans should be done with caution.
PRE-EXERCISE EVALUATIONS
Exercise testing is not required for survivors who plan to participate in low- to moderate-intensity activities such as walking, flexibility exercises, or resistance training. Prior to more vigorous-intensity exercise, survivors should follow the general ACSM guidelines for exercise testing and prescription, which may include formal clinical exercise test administration by an exercise professional for individuals at increased risk for complications associated with risk factors unrelated to cancer and/or other preexisting health conditions, such as heart disease.
The challenge for implementation of the medical evaluation is determining the thresholds for risk indicators. Exercise professionals will look to the oncology care team to provide guidance. Thus, as noted, there is a need to balance the risks associated with disease versus the risks associated with a sedentary lifestyle. Relying on a symptom-based approach is recommended when exercise recommendations and prescriptions are provided.
The ACSM guidelines for cancer survivors were intended to address cancer-related issues; they come within the broader context of conventional exercise guidelines and evaluations for managing other conditions.6,7,– The guidelines thus recommend evaluation for other conditions such as peripheral neuropathies and musculoskeletal morbidities secondary to treatment. For individuals who have received hormone therapy, evaluation of fracture risk is recommended. Survivors with known metastatic disease to the bone are recommended for evaluation, and individuals with known cardiac conditions should receive a medical evaluation per existing guidelines.7 The ACSM guidelines suggest that exercise professionals consult with the survivors' medical teams in this phase of exercise planning. As a result, the oncology professional should anticipate questions about the presence of – or risk posed by – these factors.
Additional tumor site-specific assessments are also recommended in the ACSM guidelines. Breast cancer survivors should have arm and shoulder morbidity assessed. Prostate cancer survivors, in particular, require evaluation of muscle strength and wasting. Colon cancer survivors who have an ostomy need to have established practices for the management of infection in place before undertaking an exercise program. Morbidly obese survivors may require additional medical clearance and supervision for exercise due to weight-related risks. This may be particularly pertinent for the endometrial cancer survivor population.
The ACSM guidelines for survivors suggest a pre-exercise evaluation for fracture risk in survivors on hormone therapy. NCCN treatment guidelines for men with prostate cancer who are on hormone therapy (androgen deprivation therapy [ADT]) recommend screening and treatment for osteoporosis according to the general National Osteoporosis Foundation guidelines.23 It is suggested that fracture risk be assessed using the World Health Organization Fracture Risk Assessment Tool (FRAX), with ADT considered as equivalent to secondary osteoporosis. NCCN prostate cancer guidelines, as well as Medicare guidelines, recommended treatment for those with a 10-year hip fracture risk of at least 3%, or a 10-year major osteoporosis fracture risk of at least 20%.,25 While NCCN breast cancer treatment guidelines recognize that certain treatments (eg, aromatase inhibitors [AI]) increase fracture risk, and women may require treatment (eg, with bisophosphonates), no guidelines for fracture risk evaluation are provided. However, the bone-health guideline note “The NCCN Clinical Practice Guidelines in Oncology: Breast Cancer and Prostate Cancer” recommend that patients for whom planned therapy includes medications that lower sex steroids should be evaluated at baseline and with periodic follow-up dual-energy x-ray absorptiometry (DXA) scans to evaluate risk of fracture.” The US Preventive Service Task Force guidelines recommend bone-density screening for all women aged 65 years and older and for women aged 60 to 64 who are at high risk for bone loss. American Society of Clinical Oncology (ASCO) guidelines suggest bone-density screening for women with breast cancer who have high-risk factors such as a family history of fractures, body weight less than 70 kg, and prior nontraumatic fracture; for postmenopausal women of any age receiving AI therapy; and for premenopausal women with therapy-induced ovarian failure. NCCN guidelines recognize that bone-density evaluation via DXA poses some challenges and risks, and thus recommends assessment using the FRAX algorithm in survivors who are at increased risk for bone loss and fracture. No fracture risk level has been defined as indicating that exercise is unsafe. ACSM exercise prescription guidelines also provide guidance on exercise in osteoporotic individuals. Finally, multiple myeloma survivors should be treated as if they were osteoporotic, given that some proportion of these survivors will have bony lesions that place them at high fracture risk.
Loss of muscle strength and wasting may be issues for some cancer survivors. The ACSM guidelines note that this is particularly so for prostate cancer survivors who may lose muscle mass during ADT. Given the exercise pathology expertise of certified exercise specialists and physical therapists, oncology care providers should feel comfortable referring assessment of strength and wasting to these individuals. However, there is not sufficient reason to send every prostate cancer survivor for such an evaluation, particularly if the men desire to begin walking or using a stationary bicycle, both of which are lower-risk activities. Criteria for defining weakness and wasting are not given in the ACSM guidelines. It is not clear under what circumstances weak individuals should avoid exercise; in fact, weakness in cancer survivors may be seen not as a contraindication to exercise, but as an indication for exercise as a therapeutic intervention, although it should be started slowly and should progress slowly, in line with the “as able” approach to physical activity recommended in the ACSM/American Heart Association physical activity recommendations for older adults.
To ensure survivor safety, the ACSM guidelines for cancer survivors recommend that survivors undergo neuropathy evaluation prior to initiating an exercise program. Neuropathy can range from mild to severe, with most survivors initially experiencing sensations of tingling, pain, or numbness. Survivors often complain of walking difficulty and of dropping items, both of which can pose safety risks in an exercise setting. Chemotherapy-induced peripheral neuropathy (CIPN) manifests as sensory symptoms (eg, numbness or tingling), cold sensitivity, and pain. Diagnostic features of CIPN include symmetrical, distal, length-dependent, “glove-and-stocking” distribution; predominantly sensory symptoms (especially pain), both in frequency and severity, rather than motor symptoms; onset after the administration of chemotherapy, which may be progressive, rapid, or “coasting”; and dose dependent. Survivors who report CIPN symptoms should begin with a supervised exercise program, such as the one offered by the LIVESTRONG at the YMCA program (http://www.livestrong.org/What-We-Do/Our-Actions/Programs-Partnerships/LIVESTRONG-at-the-YMCA), currently available in 17 states, to manage survivor safety. Survivors may also benefit from choosing an activity with greater stability relative to other activity options, such as riding a stationary bike rather than walking. Exercise professionals are best equipped to make exercise prescriptions in this scenario.
Arm and shoulder morbidities may make some types of exercise less safe, particularly for breast cancer survivors who are at increased risk for arm and shoulder morbidities even in the absence of exercise. As a result, prior to the patient's beginning an upper body exercise program, an evaluation for range of motion, scapular stability issues, weakness, pain, and lymphedema is of value. Ideally, such evaluations would be done by a lymphedema specialist with the level of training recommended by the National Lymphedema Network.30 However, the inability to access such expertise should not be translated into avoiding exercise for the upper body. Even in the absence of any upper body morbidity evaluation, exercise for the upper body can be started at a very light intensity and progressed according to symptom response. Again, survivors may benefit from a supervised program in the community, physical therapy, or a clinical exercise-specialist setting. There is tremendous value to establishing clear links from community-based exercise programs back to the clinical rehabilitation medical profession so that if any problems arise, breast cancer survivors can be easily referred and treated so they may return quickly to exercise.
CONTRAINDICATIONS TO EXERCISE
In addition to the need for pre-exercise evaluations in some survivor groups, the ACSM guidelines specify some conditions in which exercise is contraindicated. These include extreme fatigue or anemia, initial wound-healing following surgery, in cases of cardiopulmonary disease, and when survivors experience noticeable changes in swelling, such as during lymphedema. Certain types of exercise might also be contraindicated in survivors with ostomies. The ACSM guidelines also exist within a context of existing clinical treatment and supportive care guidelines, which address overlapping indications. Thus, we believe that successful implementation looks at the totality of expertise available in the cancer care community.
NCCN guidelines recommend that certain survivor groups (eg, patients with comorbidities, recent major surgery, functional or anatomical deficits, or substantial deconditioning) obtain referral to physical therapy to facilitate exercise during fatigue. NCCN guidelines offer tools for the evaluation of fatigue, such as the Functional Assessment of Cancer Therapy–Fatigue (FACT-F) instrument, with thresholds for defining extreme fatigue (eg, a score of 7–10 in response to a general, single-question, self-reported fatigue rating).31 It is also important to note that initiation of an exercise program is a recommended treatment (category 1 level evidence-high level evidence and uniform NCCN consensus) for fatigue in the NCCN fatigue guidelines. The ACSM guidelines state that “it is reasonable to encourage all patients to engage in a moderate level of physical activity during and after cancer treatment,” and they note that survivors may require referrals to exercise specialists. NCCN guidelines indicate that exercise should be used with caution in survivors with bony metastases, thrombocytopenia, anemia, fever, active infection, or limitations due to metastases or other illness. While not all conditions are explicitly noted in the ACSM guidelines, this symptom-based approach to proceeding with caution – beginning at a low-intensity level and progressing slowly as survivors are able – is consistent with the ACSM guidelines approach.
NCCN guidelines define anemia as hemoglobin (Hb) no greater than 11 g/dL, or at least 2 g/dL below baseline, but the NCCN guidelines do not give a definition for extreme anemia.31 At present, there are no data to indicate that low- or moderate-intensity aerobic exercise, such as walking, is unsafe in survivors with (nonextreme) anemia, and one study indicates that it is safe in mildly to moderately anemic survivors. As noted, implementing thresholds in such a setting may keep cancer survivors from accessing the myriad benefits that exercise can offer. However, oncology providers should make survivors and their exercise professionals aware of symptoms (eg, sustained tachycardia, chest pain, dyspnea on exertion, or syncope) that may indicate an increase in risk and suggest the need to temporarily suspend exercise until the anemia is treated. Symptoms may appear below common severe anemia thresholds (eg, at less than 8 g/dL) and as such, a symptom-based approach to anemia-associated exercise risks may be preferable.
ACSM guidelines caution that survivors should allow adequate time to heal after surgical treatments. The time and clinical indicators that define “adequate” will clearly vary by type of surgical procedure (eg, open versus laparoscopic) and the survivor's presurgical health. At the time the survivor is cleared to resume normal activities of daily living, the survivor should be counseled to begin a progressive exercise program. Survivors who have an ostomy should be counseled to avoid contact and water sports, but can safely participate in many forms of exercise, including brisk walking and cycling. These survivors should also take care to avoid excessive intra-abdominal pressure. Survivors with ostomies are also indicated to get physician clearance before engaging in weight training because of the risk of herniation. Clinicians may want to suggest that survivors with ostomies begin with supervised resistance exercise, particularly if they have not previously been active.
Individuals with cardiac conditions that contraindicate exercise, regardless of their cancer survivorship status, should be counseled accordingly. However, many cardiac patients can safely exercise, and guidelines have long been in place to direct exercise testing and prescription in this population.7
If survivors, regardless of tumor site, begin to experience swelling, they should stop exercising and seek medical treatment for the swelling. Evidence indicates that breast cancer survivors with lymphedema can safely exercise, including resistance training, with proper compression, and that such exercise does not cause lymphedema in women at risk for the condition., However, there are limited parallel data in individuals with lower extremity lymphedema secondary to cancer treatment. Home exercise programs have been found to be a useful adjunct to physical therapy programs for treating arm and shoulder morbidities in breast cancer survivors.
In general, there is a limited amount of evidence on which to issue specific guidelines on contraindications and precautions to exercise. As noted by Wolin et al, the implementation of survivor programming in the absence of conclusive evidence is a necessary reality, and clinicians will make judgments based on their previous clinical experience. However, the key conclusion of the ACSM guidelines on exercise for survivors is that exercise is safe and offers a multitude of benefits. There are survivor groups who require modifications to the general guidelines, particularly for resistance training. For example, adults who have undergone human stem cell transplant (HSCT) will initially require a lighter intensity and slower progression. Moreover, morbidly obese cancer survivors, as is common in endometrial cancer, may also require greater supervision. Colon cancer survivors with a stoma may need to start at a low resistance and progress slowly to avoid herniation. Hematologic and prostate cancer survivors may otherwise follow the PAGA. For gynecologic cancer survivors, data on the safety of resistance training in women with lower limb lymphedema do not exist, and survivors should proceed with caution. In breast cancer, women are recommended to begin with a supervised program and progress slowly at low resistance.
PRESCRIPTION AND REFERRAL
In providing an exercise prescription to cancer survivors, the risks of inactivity must be balanced against the risks of activity. As such, at the very least, oncology clinicians should counsel survivors to “avoid inactivity.” However, many survivors will seek a greater amount of guidance and prescription from their clinicians to achieve the health benefits offered by activity. While exercise specialists, including physical therapists and ACSM Certified Cancer Exercise Trainers, are best equipped to provide such a prescription, geographic or financial access to these specialists should not serve as a barrier to exercise. For example, walking – particularly when begun at a low level and progressing to a moderate pace – is a safe activity for most cancer survivors. Similarly, the use of a stationary bicycle or cycle ergometer allows for stable and safe exercise that can progress as an individual's functional capacity allows. For survivors who require supervision or who may need guidance on safe procedures, referral to a local physical therapist or exercise specialist can help. The ACSM allows individuals to search for those certified through its programs,37 although other local programs may also exist. When evaluating a local program, survivors and oncologists should look for those that (1) have a familiarity with cancer treatment side effects and late effects; (2) rely on a program that progressively increases dose, duration, and intensity as tolerated; (3) include detailed regular attention to infection control practices; and (4) are delivered by certified exercise professionals. While finding a program run by those with the ACSM cancer exercise specialist certification may be difficult, those with an ACSM or ACE certification as a trainer or exercise professional should be considered a minimum. For example, the YMCA has partnered with the LIVESTRONG organization to offer programs specifically for cancer survivors in many communities. In addition, the Cancer Support Community organization offers exercise programs at many of its cancer survivor centers. Many comprehensive cancer centers are affiliated with universities or hospitals that have fitness facilities where staff may have experience working with cancer survivors as a function of their proximity to this survivor population. When referring survivors to any exercise specialist or facility, physicians should suggest that survivors inquire about the exercise practitioner's experience working with cancer survivors. Certifications like that offered by ACSM for cancer specialists are an excellent indication of this experience.
The implementation of guidelines into clinical practice is challenging because the guidelines do not deal with the many logistical issues that arise in clinical practice, which points to the fact that this is an evolving field with substantial research gaps. The limits on where the existing guidelines can be extrapolated are presently unclear, and clinicians will necessarily need to draw on their previous experiences to decide where this is reasonable and where it is not. Similarly, the ACSM guidelines do not vary the exercise prescription based on the end point of interest, largely because the data are not sufficient to allow for it, though this is certainly something that future iterations of the guidelines may consider. However, exercise guidelines have historically focused on a prescription that yields the most benefits, even if some benefits may be obtained with lower or higher doses. Finally, the ACSM guidelines do not provide specific data on alternative types of activity, such as yoga or Zumba, because sufficient data were not available to evaluate them, and this remains an area for greater study.
CONCLUSION
First and foremost, cancer clinicians should remember that exercise is safe for most cancer survivors and does not interfere with their ability to complete or benefit from medical treatments. Moreover, exercise offers many health benefits to cancer survivors, many of whom remain at increased risk for other chronic diseases including diabetes and heart disease. Efforts to help survivors avoid inactivity and progress to meeting the PAGA's recommended levels of activity are key to their long-term physical and psychological health. Exercise testing and prescription are best done by exercise professionals or physical therapists in consultation with the cancer care team. Exercise professionals can best do their job when information on survivors' health and treatments are available. That said, many survivors can safely begin a low- to moderate-intensity exercise program, such as walking, without supervision or exercise specialist evaluation. Oncology care professionals play an important role in promoting exercise programs during and after cancer treatments. Despite gaps in the literature that informed the ACSM guidelines, oncology professionals should feel comfortable prescribing exercise to cancer survivors, with advice to start with light-intensity exercises, to progress slowly, and to allow the survivors' symptoms to guide the process.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.